Challenges in Biopsies
There are various types of urological cancers, the most common ones being prostate and kidney cancer. In cancer, early and accurate detection significantly improves survival rate and reduces treatment cost. Similar to other cancers, detection is performed using a biopsy – inserting a needle to the suspicious tissue and sampling it. Often there is uncertainty regarding exact positioning, so the tissue is penetrated several times to verify adequate sampling.
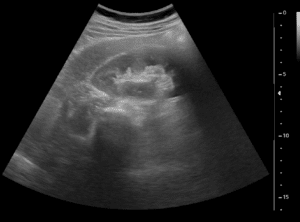
The biopsy is performed with ultrasound (US) guidance – real-time imaging for needle tracking and tissue visualization. However, ultrasound limitations include poor image resolution and high variability among users, making it very difficult to ascertain the exact position of the needle and the correct scatter of samples.
Current diagnosis protocol when suspicion of cancerous tumors in the urological tract arises, requires a CT or MRI scan. These scans provide high-resolution 3D data of the anatomical regions, which allow visualization of the lesions within the urological tract.
Segmentation and 3D reconstruction from CT/MRI
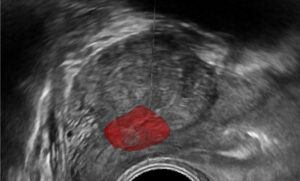
Recent developments in computer vision and AI allow accurate segmentation of desired organs and lesions within. Neural networks can be trained to segment the organs within the urological tract, and even sub-organs within them. Also, lesions or tumors can be segmented, resulting in a 3D model of the patients relevant urological system, with the interesting regions segmented and highlighted. This model is actually a custom map of the patient.
Biopsy Planning
The biopsy requires prior knowledge of where the organ is located (e.g. prostate), where the suspected lesion is within the organ, and what is the least harmful direction to get to the lesion (without damaging nearby structures). In real-time the physician uses his experience and Ultrasound guidance to perform this task accurately, but all this information exists in the CT/MRI data!
Based on the scan and the segmentations, the best path from the skin to the lesion can be determined, automatically or by the physician. The system can then extract the exact point of penetration on the skin, the ideal angle of the needle, and the distance from skin to the lesion which the needle needs to penetrate. The physician can use these directions as a baseline for the biopsy and be certain that the needle is pointing in the right direction.
Additional modules can use Ultrasound or X-ray for needle tracking. The probe position can be tracked using stereo cameras or freehand sensors on the probe, and this position can be used to verify needle position. Needle distance from skin can be calculated using the Ultrasound/X-ray calibration and needle tracking, so that the physician knows exactly how deep the needle is penetrating. All these tools can improve the procedural accuracy and reduce time and error-rate.
RSIP Vision Can Help You Plan Your Procedure
Training a network to accurately segment objects, render these into a 3D model, and add this capability as a tool for procedure planning requires advanced knowledge and experience in computer vision. Our team at RSIP Vision consists of engineers and clinicians with vast experience in this field, and a proven track-record with similar modules. We can add this tool to your portfolio rapidly and efficiently, and help you speed your time to market.


 Urology
Urology