Larger stones in the kidney and proximal ureter need to be treated with PCNL (Percutaneous Nephrolithotomy), a minimally invasive urology procedure intended to remove them. It is today a very effective procedure, as it can be operated via a relatively small opening with a reduced time of hospitalization. There is also a version of it called mini-PCNL, a tubeless procedure with an even smaller port of entry, while maintaining a similar rate of efficacy.
More surgeons would be able to perform PCNL if the access part were made simpler. That is one of the most challenging parts: it starts at the moment of the initial puncture until a path is created from the skin to the kidney itself in the correct location. That would make the surgeon’s learning curve improve faster and at the same time more post-op complications could be avoided. As things stand today, the surgeon takes all decisions regarding the access out of his experience and judgement, aided by fluoroscopy or ultrasound.
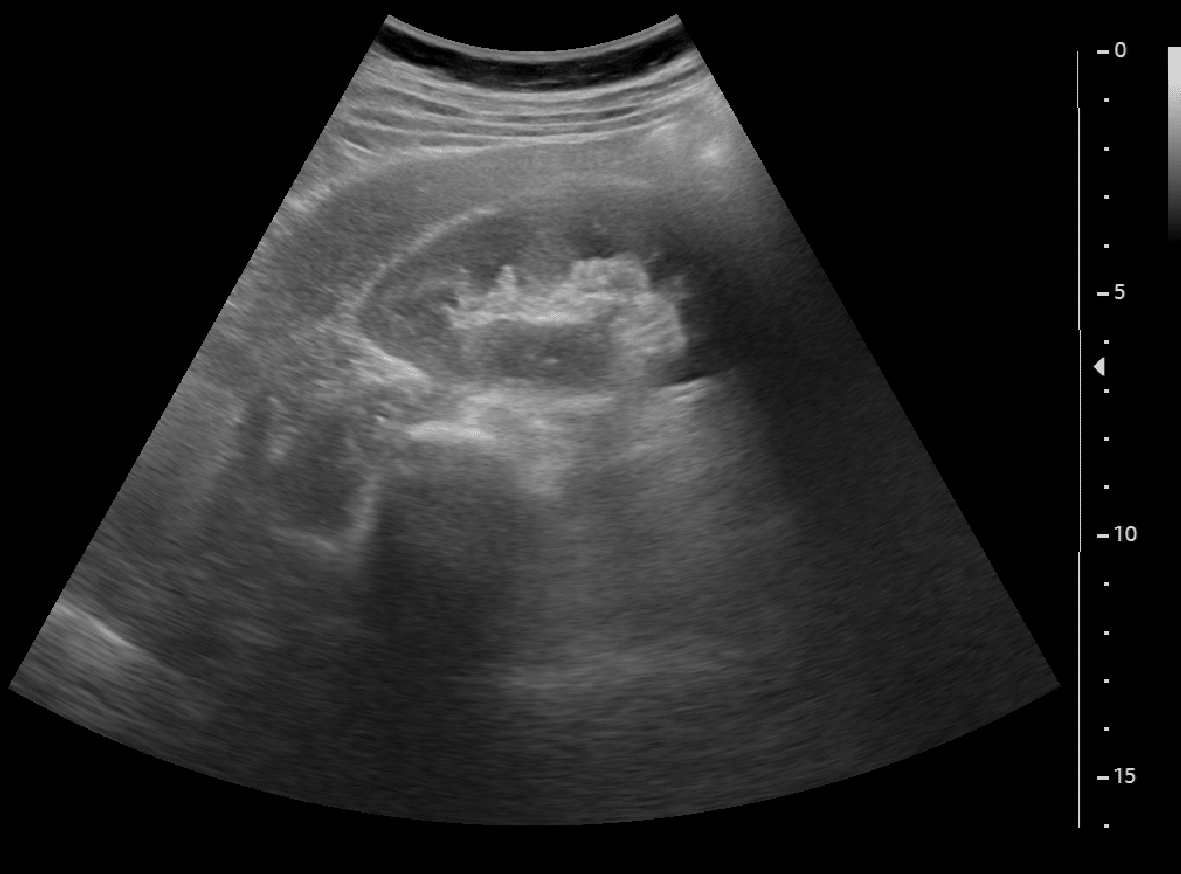
The intervention can be delivered when the patient is prone (lying on the stomach), which is quite challenging for anesthesia; or supine, when the patient is face up, which is simpler. When the needle is inserted in the kidney, the surgeon may be assisted by fluoroscopic guidance to perform the best possible needle insertion – the right angle and the tracking of the needle during the insertion; when ultrasound guidance is preferred to avoid radiations, some more dexterity is required from the surgeon, since less of the anatomy is visible. At the end of the procedure, the surgeon might choose a tubeless or fully tubeless solution, which avoid the insertion of a catheter to serve as a drain (nephrostome) for just a few days.
This procedure is quite common and successful. It is possible though to improve it. In particular, we suggest to improve the access part of PCNL. Access is one of the most challenging parts of the procedure, and we believe that dramatic improvements can be made by integrating artificial intelligence solutions combined with hardware. This will procure better outcomes and easier procedures even for less experienced surgeons. Less punctures will be needed since the number of incorrect accesses, involving removing the needle and puncturing again, will be much lower. Less punctures lead to less complications in the way.
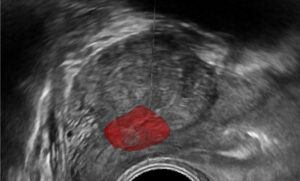
The surgeon must choose very carefully the access route for the needle. How can we ask Computer Vision and AI to improve this choice? The first improvement is in the planning part: the surgeon can look at the CT and select – based on his/her experience – the best way to puncture, from which part of the body and to which calix. The choice lays with the expert, which AI can assist but not replace, of course. AI algorithms can also help during the procedure itself. Using special tools, it can show where the needle is, where the calices are, and whether the trajectory is correct according to the plan. It is crucial that the needle is inserted into the right calix. When the surgeon uses fluoroscopy, computer vision analysis sees the needle from different angles and combines the views into one and conveniently communicates this information to the surgeon, assisting him/her to make sure that the access is done correctly. When the surgeon uses ultrasound, the image is not straightforward to interpret. In this case too, AI assists the surgeon to make informed choices.
How AI does this? There are a few tools that can be built using AI. The first one is segmentation of the region, of the needle, of the kidney itself. Additionally, computer vision can merge two images taken with fluoroscopy and provide 3D information: what would be complicate for the mind is made much easier by mathematical formulas. When we have additional external hardware like electromagnetic trackers (EMT) or optical trackers, we can add this information and compute the position of the needle, even when it is not clearly visible in the image itself. We can also fuse all this information to provide additional assistance to the surgeon. If the needle is beneath the ultrasound plane, this info will guide the surgeon to point the ultrasound probe in a better direction.
This is improved PCNL with Computer Vision. AI algorithms are the work of expert engineers: providing correct information to the surgeon is a major concern and any misleading info about the exact location of the needle is potentially dangerous. AI and the surgeon do not replace one another: they should complement each other and work together. The key contribution of AI is in the detection of relevant anatomical structure and the needle, in the mathematical formulas for 3D fusion and in the combination of 3D data coming from external sources, like an EMT or Multiview fluoroscopy images. Contact RSIP Vision to learn more.


 Urology
Urology