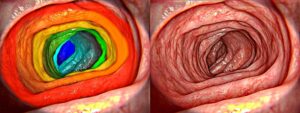
While ultrasound imaging cannot be replaced, adding Intravenous OCT to endoscopy procedures significantly improves image resolution and increases the ability to detect plaque and segment it.
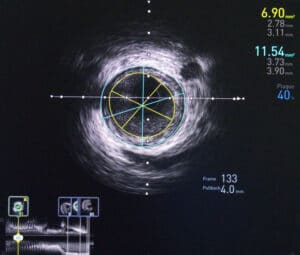
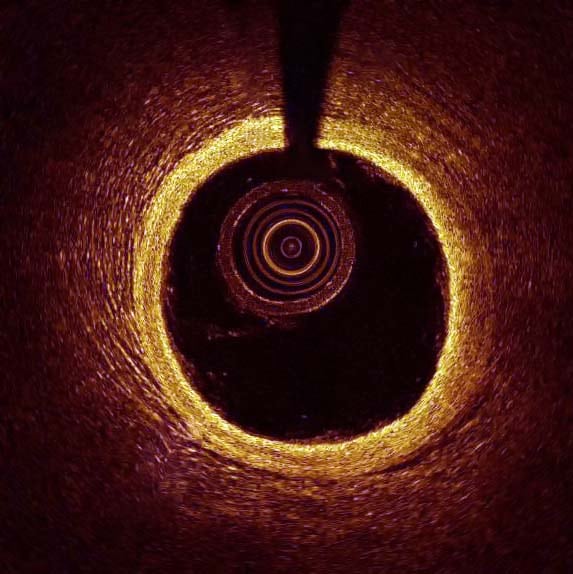
Intravenous Optical Coherence Tomography (IVOCT) is a catheter-based medical procedure which uses a near infra-red light to examine the invitro vascular wall structure. Its ability to reach high-resolution – around 10 microns – means it is able to detect very thin layers of plaque in veins, layers which the 150-200 micron resolution of regular ultrasound usually misses. Images acquired using intravenous OCT, have been analyzed successfully using classical techniques such as support-vector machines. However, deep learning and convolutional neural networks (CNN) are required to get the most out of these images; with them, accuracy of over 90 per cent can be achieved.
Despite its high resolution, when comparing penetration depth intravenous OCT, which has only a 1-2-millimeter penetration range, falls short of ultrasound. Each imaging modality has different strengths, and best results are achieved when using a combination of both. We maximize our detection capabilities by using image registration to align the two scans so that they represent the same exact area and position. From there a neural network analyzes each image offline and uses the best results from each.
Ilya Kovler CTO at RSIP Vision adds: “From my experience, the high degree of speckle noise in OCT images can hamper the plaque segmentation task. Therefore, adding a pre-processing stage to reduce this noise is critical to the success of the segmentation.”

 Endoscopy
Endoscopy