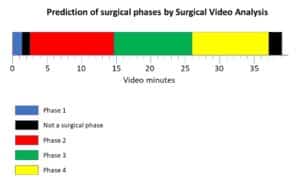
The work load can be reduced by introducing an accurate efficient aid for each procedure, relieving the time burden in surgery planning and performance. Emerging technologies have completely altered the course of orthopedic surgery planning, simulation, and performance. Orthopedic surgeons can now benefit from the use of a mature set of computer vision tools for patient-specific measurement, navigation, surgical simulation, surface reconstruction, and implant design. Bringing point and surface registration in the field of orthopedics, computer vision and image processing hold the potential to improve surgical practices and affect surgery outcome to favor the benefit of patients and fast recovery.
Semi-automated registration in orthopedics
Oftentimes a surgeon is required to register between a patient’s bone to a pre-operative bone or implant model. This can be performed by marking corresponding areas in both. In a common scenario, the surgeon chooses well-defined locations on both bone and model. These fiducial points are either mechanically or optically marked to be able to deduce the rigid transformation needed for registration.
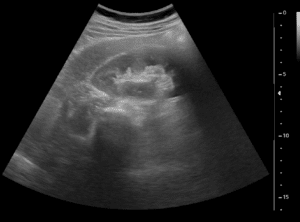
Measurement accuracy being a strict constraint to registration algorithms. As a matter of fact these algorithms are expected to operate for total knee replacement within less than 1 mm accuracy. Many registration algorithms have been proposed to meet the accuracy restriction for a given imaging modality (MRI, CT or ultrasound) and have been incorporated into routine surgery planning procedures.
Measurement errors in finding fiducial points can be overcome via statistical means, by which a rigid transformation is estimated based on the most probable location of fiducial markers. Once registration accuracy has been properly met, precise measurement can then follow by combination of image processing and mathematical modeling of the measured bone.
Early registration in orthopedics implemented simple paired point matching. These algorithms relied on a simple solution of a mathematical relationship between points but yielded insufficient accuracy. Coupled with surface matching, the accuracy of registration was improved. However, both techniques did not receive wide clinical acceptance. Other approaches include the calibration of (intraoperative) fluoroscopic and ultrasound images by feature and point intensity-based matching. Trade-offs for registration should include, in addition to accuracy, the feasibility of acquiring landmark points for registration in a minimally invasive and radiation-free manner.
In total knee replacement, implant design needs to reach an alignment error of less than 3 degrees. These requirements have been empirically found to prevent long-term implant wear and allow more satisfactory function. Computer-based alignment systems now address these restrictions by robust registration and accurate surface reconstruction. With advances in surface modeling and the ability to match a flexible surface model to observable fiducial points, reconstruction of an accurate surface for implant design is increasingly utilized in clinics.
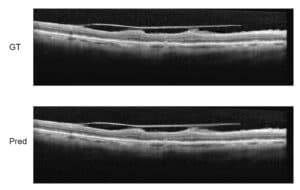
A correct match between imaging modalities and the fabricated implant is crucial for the short and long-term success of orthopedic surgeries. With the increased incorporation of computer-vision and image processing techniques into the surgical planning and simulation process, the likelihood of success is on the rise. For these ends, computerized measurement tools have been constructed to perform crucial measurements. Semi or fully automated measurement tools have been constructed successfully by engineers of RSIP Vision for over two decades. At RSIP Vision, we build computer vision based tools for measurement in both medical and non-medical applications, always adhering to the strictest accuracy standards.