Navigation systems in orthopedic procedures are now an integral part of the preoperative and intra-operative process. Advances in vision-based medical technologies, such as X-ray and CT, have completely transformed orthopedic surgery planning and operation procedures. Newly introduced technologies, such as the c-arm-CT extend the output of visual information from spatial 2-D fluoroscopy into volumetric data. The enrichment in data acquired opens up new avenues in preoperative treatment, for example in fracture reduction, allowing minimally invasive manipulation of bones, insertion of nails and screws, and radiation dose reduction during fluoroscopy, by displaying real-time virtual anatomical models. Thus, integration of advanced vision algorithms into imaging devices are not only useful for patient and staff safety but also enable the formation of a rational framework for orthopedic navigation, planning and decision making.

Fractures in long bones such as the thighbone (femur) injuries are typically related to road accidents but are also common in falling injuries, among elderly population and people with vitamin D deficiency (hip fracture). 300,000 hip fractures are annual treated in the United States and 6 millions worldwide. In high impact injuries it is common for the fracture to result in a noticeable separation into two segments of the femur. Surgery in such cases requires initial alignment of the proximal and distal parts of the broken bone, followed by insertion and securing of a nail in the inner shaft of the proximal bone (medullary cavity).
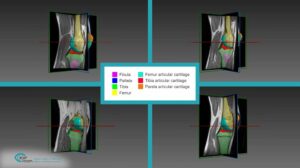
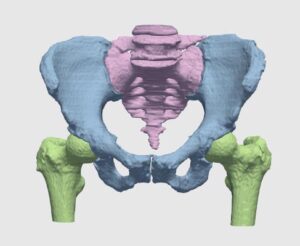
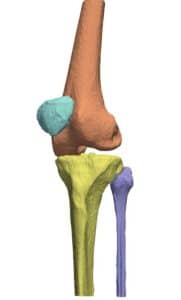
Bone alignment procedure utilizes fluoroscopic image for pose estimation and guidance of the robotic surgical assistants. Following a registration procedure (see Point and surface registration in orthopedy), the volumetric data is used to construct a 3D bony structure of the femur (as will be explained in an upcoming article about 3D reconstruction in orthopedic surgery by RSIP Vision) and indicate bone pose (position and orientation). In short, image features are matched to a pre-designed flexible geometrical model of the bone, in a top bottom approach involving optimization; this generates a registered virtual model of the femur’s segments. Computational models for fracture alignment have been shown to increase the accuracy and reduce complication resulting from segment misalignment, which amount for about 20% of femur fracture complications.
Computer vision approaches for 3D reconstruction of the femur are done on an individual case basis. It can therefore be considered as personalized medicine, as patient specific parameters are used to calibrate a bone model that is used to guide the physician in the alignment process. The volumetric nature of the data reduces the need for the physician to mentally reconstruct the fracture region to deduce the best pose.
Bone alignment procedure utilizes fluoroscopic image for pose estimation and guidance of the robotic surgical assistants. Following a registration procedure (see Point and surface registration in orthopedy), the volumetric data is used to construct a 3D bony structure of the femur (as will be explained in an upcoming article about 3D reconstruction in orthopedic surgery by RSIP Vision) and indicate bone pose (position and orientation). In short, image features are matched to a pre-designed flexible geometrical model of the bone, in a top bottom approach involving optimization; this generates a registered virtual model of the femur’s segments. Computational models for fracture alignment have been shown to increase the accuracy and reduce complication resulting from segment misalignment, which amount for about 20% of femur fracture complications.
Computer vision approaches for 3D reconstruction of the femur are done on an individual case basis. It can therefore be considered as personalized medicine, as patient specific parameters are used to calibrate a bone model that is used to guide the physician in the alignment process. The volumetric nature of the data reduces the need for the physician to mentally reconstruct the fracture region to deduce the best pose.

 Orthopedics
Orthopedics