This page is about software developed by RSIP Vision to detect brain lesions in MRI images. If you want to boost your project with the newest technology advancements in medical imaging, request a call from our top engineers.
Lesions in the central nervous system (CNS) are aggressive and frequently fatal. Individuals diagnosed with CNS tumors often suffer from disabilities caused by dysfunctional neurological state and deterioration in systemic activity, leading to relative short expected life-span post diagnosis. Lesions of the CNS are highly variable in both position and biochemical activity, with no common origin pinpointed to date. Causes for CNS lesions range between injuries, strokes, exposure to chemical or radiation, metastases, infection, genetic abnormalities, whereas other lesions’ origin remains elusive. The World Health Organization (WHO, 2007) has classified CNS tumors into a total of more than 50 subtypes, with new entries presented annually. An estimated 80,000 new cases of primary malignant cases will be diagnosed in 2016 in the US alone, with incident rates increasing annually.
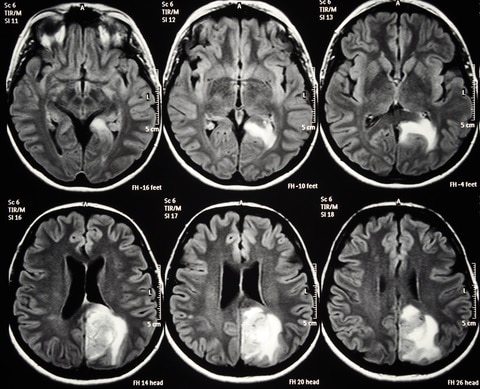
Brain lesion detection is most commonly performed by Magnetic Resonance Imaging (MRI). MRI enables a relative clear view of CNS tissues and distinguishes soft white and gray matter in the brain after injection of contrasting agents (gadolinium). Monitoring the characteristics of the lesion, such as its size, shape, position, together with its histological composition and rate of spread, allows oncologists to grade the tumor according to scale of severity and to decide a course of action.
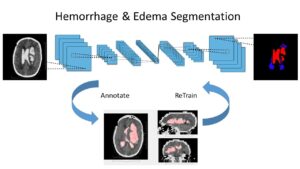
Physiological features of the tumor are an important aspect in the central nervous system since the visible size in MRI and the actual size and geometry might significantly differ. The soft matter in the brain provides means for tumors (glioblastoma, see figure above) to spread beyond the bulky sphere into a more elongated thin shape which invades surrounding tissues. Expert knowledge is required in such situations to distinguish edema from the tumor mass and estimate the invasion to neighboring tissues. According to the shape of the tumor, oncologists assess the extent of its spread to vital parts of the brain and plan a resection (when applicable) in a rational manner.
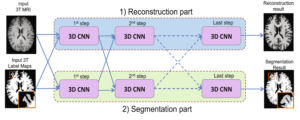
The use of imaging techniques in brain lesion detection can significantly reduce bias in diagnosis caused by oncologist subjectivity. MRI and other modalities used in practice (PET, CT, etc.) open up new opportunities for automated processes to detect, monitor, integrate information from other modalities and grade CNS lesions. Automatic computer vision and machine learning algorithms are constructed to segment MRI volumetric data into all voxels classified as lesions and all the rest, generating a binary classification problem.
Due to the unpredictable shape of the tumor, statistical shape representations are employed in brain lesion detection algorithms. Such statistical models form as shape priors to restrict segmentation in later stages. Binary classification assigns each voxel to the most probable class assuming the shape prior (Bayesian theory). Prior models can be formed by training a classifier on a group of extracted features from the neighborhood of each voxel in a training set. The actual set of feature can include intensity values as well as Haar-like features. Optimization of the segmentation based on the prior is performed by max-flow/min-cut algorithm, which is optimal for this Bayesian classification problem.
An automated approach to segment irregular 3D shapes from MRI volumetric data can greatly assist oncologists in their prognosis of CNS lesions. Automated methods based on computer vision, image processing and machine learning methodologies are highly flexible to inclusion of expert knowledge and have been demonstrated in numerous applications to perform accurately and robustly.
Cutting edge algorithms to match cutting edge applications requires the hands of experts, like RSIP Vision’s engineers and scientists. This is even truer for medical applications software.
Physiological features of the tumor are an important aspect in the central nervous system since the visible size in MRI and the actual size and geometry might significantly differ. The soft matter in the brain provides means for tumors (glioblastoma, see figure above) to spread beyond the bulky sphere into a more elongated thin shape which invades surrounding tissues. Expert knowledge is required in such situations to distinguish edema from the tumor mass and estimate the invasion to neighboring tissues. According to the shape of the tumor, oncologists assess the extent of its spread to vital parts of the brain and plan a resection (when applicable) in a rational manner.
The use of imaging techniques in brain lesion detection can significantly reduce bias in diagnosis caused by oncologist subjectivity. MRI and other modalities used in practice (PET, CT, etc.) open up new opportunities for automated processes to detect, monitor, integrate information from other modalities and grade CNS lesions. Automatic computer vision and machine learning algorithms are constructed to segment MRI volumetric data into all voxels classified as lesions and all the rest, generating a binary classification problem.
Due to the unpredictable shape of the tumor, statistical shape representations are employed in brain lesion detection algorithms. Such statistical models form as shape priors to restrict segmentation in later stages. Binary classification assigns each voxel to the most probable class assuming the shape prior (Bayesian theory). Prior models can be formed by training a classifier on a group of extracted features from the neighborhood of each voxel in a training set. The actual set of feature can include intensity values as well as Haar-like features. Optimization of the segmentation based on the prior is performed by max-flow/min-cut algorithm, which is optimal for this Bayesian classification problem.
An automated approach to segment irregular 3D shapes from MRI volumetric data can greatly assist oncologists in their prognosis of CNS lesions. Automated methods based on computer vision, image processing and machine learning methodologies are highly flexible to inclusion of expert knowledge and have been demonstrated in numerous applications to perform accurately and robustly.
Cutting edge algorithms to match cutting edge applications requires the hands of experts, like RSIP Vision’s engineers and scientists. This is even truer for medical applications software.