Diabetic Retinopathy (DR) is an eye disease resulting from long-term diabetic condition. About 80% of long-term diabetic patients suffer from some degree of DR, which accounts for more than 10% of cases of blindness in the USA alone. Early detection of DR and monitoring its progression can spare reduce the occurrence of such cases and slow down vision impairment.
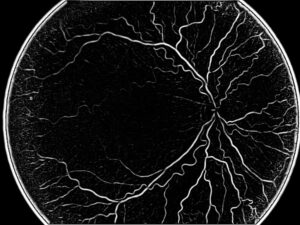
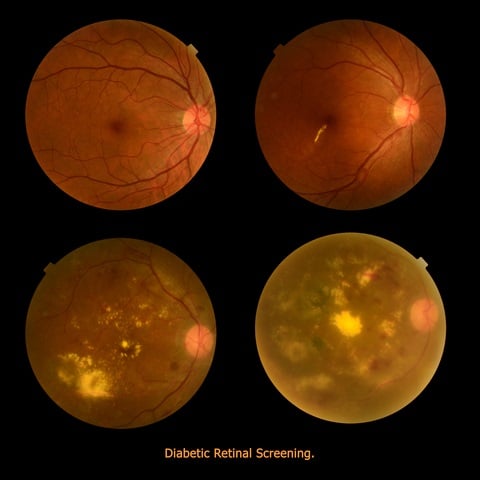
With DR, the vascular tree in the retina is damaged due to accumulation of glucose and fructose. As a result of this accumulation, hyperglycemia (high blood sugar) causes the cells wrapping the vascular walls (pericytes) to be deprived of oxygen (hypoxia). The pericytes undergo apoptosis (cell death), which thickens the vascular walls in the eye, causing vision deterioration such as blurring and the appearance of black spots in the viewing field. These lesion can be seen in fundus images as dark brownish-gray spots (see image below).
With DR, the vascular tree in the retina is damaged due to accumulation of glucose and fructose. As a result of this accumulation, hyperglycemia (high blood sugar) causes the cells wrapping the vascular walls (pericytes) to be deprived of oxygen (hypoxia). The pericytes undergo apoptosis (cell death), which thickens the vascular walls in the eye, causing vision deterioration such as blurring and the appearance of black spots in the viewing field. These lesion can be seen in fundus images as dark brownish-gray spots (see image below).
Automated tools play a significant role in monitoring the progression of patient’s Diabetic Retinopathy. This is especially true for diabetic patients suffering from this condition for a prolonged period. Disease progression is tracked over several years, where in many cases both imaging modalities as well as the treating physician have changed from the beginning of monitoring. For these reasons, robust automatic extraction of the retinal lesion positions and registration between the imaging outputs of several modalities are important. Automation enables the physician to assess the disease progression with higher accuracy and determine the course of action based on reliable past data. In addition, automatic extraction of lesion positions enables quick scanning of many images and can act as an alert system for early diagnosis of Diabetic Retinopathy.
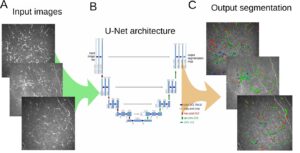
Automatic DR detection begins with the segmentation of the vascular tree in fundus images. There are several methodologies to extract the vascular tree: some common algorithms rely on initial steps of edge detection; other algorithms rely on the appearance of blood vessels against the background in fundus camera to apply morphological operations for vascular segmentation. A combination of the two approaches is of course feasible. Since the fundus camera provides 2D images, deducing the actual spatial position of vessels is a non-trivial task. Despite that, segmented vascular tree can help locate other important physiological structures such as the optical disk. The optical disk is located initially at the point of vessel convergence. Working in the framework of graphs to represent the segmented vascular trees allows us to harness the power of graph theory for characterizing the vascular tree and extracting unique positions on it such as the convergence points which help localize the optical disk. The optical disk is the stable position from which registration operation can begin.
Under the assumption of continuous change in vessel width along the vascular tree, any abrupt changes in appearance indicate potential positions of lesions. Irregularities in color and geometrical forms are good indicators for lesions positions. Their boundaries are subsequently delineated in such a way that the vascular tree is not segmented with them. Lesions in DR can appear off the vascular tree (see again the image), in which case lesion detection in fundus images is much more trivial.
For registration purposes, the vascular tree does not necessarily need to be segmented. Rather, only key features should be extracted and compared between images to allow scaling and alignment of both images. Such features can be the position of the optical disk and the position of the intersection of vessels.
In the age of modern medicine, harnessing the power of computer vision algorithms for quick and robust detection of abnormalities benefits both the physician and patients. Quick scanning of hundreds of images and automatic alignment and analysis reduces the burden imposed on physicians. On the other hand, the ability to quickly integrate information and present it concisely enables physician to arrive at the right clinical decision which facilitates effective patient prognosis. At RSIP Vision we push computer vision technology further by developing cutting edge algorithms for medical applications. Talk with our consultants to learn how we can help you on your projects.
Automatic DR detection begins with the segmentation of the vascular tree in fundus images. There are several methodologies to extract the vascular tree: some common algorithms rely on initial steps of edge detection; other algorithms rely on the appearance of blood vessels against the background in fundus camera to apply morphological operations for vascular segmentation. A combination of the two approaches is of course feasible. Since the fundus camera provides 2D images, deducing the actual spatial position of vessels is a non-trivial task. Despite that, segmented vascular tree can help locate other important physiological structures such as the optical disk. The optical disk is located initially at the point of vessel convergence. Working in the framework of graphs to represent the segmented vascular trees allows us to harness the power of graph theory for characterizing the vascular tree and extracting unique positions on it such as the convergence points which help localize the optical disk. The optical disk is the stable position from which registration operation can begin.
Under the assumption of continuous change in vessel width along the vascular tree, any abrupt changes in appearance indicate potential positions of lesions. Irregularities in color and geometrical forms are good indicators for lesions positions. Their boundaries are subsequently delineated in such a way that the vascular tree is not segmented with them. Lesions in DR can appear off the vascular tree (see again the image), in which case lesion detection in fundus images is much more trivial.
For registration purposes, the vascular tree does not necessarily need to be segmented. Rather, only key features should be extracted and compared between images to allow scaling and alignment of both images. Such features can be the position of the optical disk and the position of the intersection of vessels.
In the age of modern medicine, harnessing the power of computer vision algorithms for quick and robust detection of abnormalities benefits both the physician and patients. Quick scanning of hundreds of images and automatic alignment and analysis reduces the burden imposed on physicians. On the other hand, the ability to quickly integrate information and present it concisely enables physician to arrive at the right clinical decision which facilitates effective patient prognosis. At RSIP Vision we push computer vision technology further by developing cutting edge algorithms for medical applications. Talk with our consultants to learn how we can help you on your projects.

 Ophthalmology
Ophthalmology